The health care needs of older people tend to be marginalised because South Africa’s health policy is focused on children, youth and maternal care. The traditional extended family system has eroded in much of sub-Saharan Africa, leaving many older people who traditionally depended on this support vulnerable. In rural households, young people often migrate to cities in search of employment. International emigration and the pandemic of HIV/AIDS have also taken their toll.
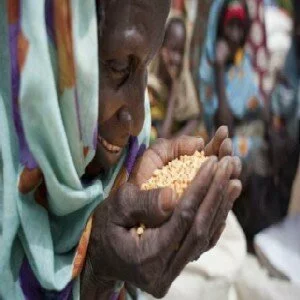
The effect is that older people lack the financial and other resources to take care of themselves. As a result, many find it difficult to meet their nutrient requirements. South Africa has the highest percentage of older people on the continent. Around 4.1 million people, or 8% of the population, are aged 60 or older and classified as pensioners. This is projected to nearly double to seven million (9.3% of the population) by 2030.
The health care needs of older people tend to be marginalised because South Africa’s health policy is focused on children, youth and maternal care. In particular, the nutritional needs of this age cohort is not being addressed with major implications for their overall health. Apart from lunch clubs at senior citizens’ centres and meals-on-wheels services, nutrition programmes for older people are sparse. So what can be done?
Why the over 60s are more at risk
South Africa’s health care services are not keeping up with the needs presented by older people who are more prone to a range of ailments and health challenges. These include: Hypertension, heart disease and stroke, all of which are on the rise.
A decline in physical and mental function. These may include dementia, depression, delirium, vision problems, poor oral health and disease – either acute or chronic. Social factors that contribute to these are isolation and loneliness, poverty and lack of access to an adequate food supply, and, in some cases – particularly in bereaved widowers – inadequate knowledge about food preparation.
The way the body digests and absorbs nutrients changes with age. This results in an increased need for calcium, vitamin D and some B vitamins.
More frequent falls and fractures. Falling can have devastating effects on functional ability. A Cape Town survey found that 26% of older people had fallen in the 12 months before the study. Another 14% sustained a fracture. Almost half of those who fell did not return to their previous level of independence.








No Comments